Healthcare organizations face mounting pressure to protect patient data while managing limited budgets and resources. Recent breach statistics reveal a troubling pattern: while healthcare providers submit the majority of breach reports to HHS, third-party vendors account for the overwhelming majority of compromised patient records. Understanding where vulnerabilities exist and how to address them has never been more critical.
The Third-Party Vendor Problem
Statistical analysis from breach reporting data shows that business associates represent a disproportionate risk. Although vendors submit only a fraction of total breach reports, they’re responsible for roughly two-thirds of all breached records. When non-regulated entities handling medical data are included, that figure climbs even higher.
This disparity highlights a fundamental compliance gap. Healthcare organizations invest heavily in securing their own networks while inadvertently trusting critical patient data to vendors whose security postures may be inadequate or unknown.
Strengthening Vendor Oversight
Effective vendor management requires three core practices:
Pre-Contract Due Diligence: Before signing agreements, organizations must thoroughly vet potential business associates. This includes reviewing documented security policies, procedures, and risk assessments. A robust business associate agreement forms the foundation, but contractual language alone provides insufficient protection.
Ongoing Monitoring: HIPAA doesn’t mandate specific audit schedules, but a risk-based approach is essential. Organizations handling large volumes of electronic protected health information (ePHI), those with incident histories, or vendors presenting other risk indicators warrant annual reviews at minimum. More frequent assessments may be necessary based on risk profiles.
Accountability Structures: When breaches occur at vendor sites, the Office for Civil Rights (OCR) holds covered entities responsible. Organizations cannot outsource accountability. Business associate agreements should require vendors to provide timely breach information and support, but the covered entity must own patient communications.
Hidden Compliance Risks in Web Infrastructure
Website security represents an often-overlooked vulnerability. Misconfigured web properties can create HIPAA violations when they result in unencrypted transmissions. Contact forms, patient portals, tracking software, and unsecured data transmission all present potential exposure points for ePHI.
Both the Privacy and Security Rules apply to web infrastructure. Organizations need initial compliance reviews focusing on HIPAA-specific risks such as encryption requirements, secure transmission protocols, and privacy notices. Technical penetration testing and remediation typically require specialized IT security expertise.
The State Law Compliance Gap
Many healthcare organizations operate under the mistaken assumption that HIPAA represents their only compliance obligation. Federal requirements establish a baseline, but state laws frequently impose stricter standards with faster notification timelines and broader definitions of protected information.
Comprehensive data privacy laws in various states now grant consumers extensive rights over their personal data, including the ability to request deletion, opt out of data sales, and pursue private legal action following security failures. These laws create compliance requirements that extend well beyond federal HIPAA standards.
Privacy Rule Fundamentals
Three critical Privacy Rule principles demand particular attention:
Right of Access: Patients possess the right to access their medical records quickly and affordably. OCR has launched more than 50 enforcement actions specifically targeting right of access violations, signaling the priority placed on this standard. Individuals should not need to file complaints to obtain their own health information.
Minimum Necessary Standard: Healthcare organizations must limit the patient information they use, access, or share to only what’s needed for specific tasks. This principle prevents unnecessary exposure of individually identifiable information while allowing providers to perform essential healthcare functions. Implementation requires more than policy documentation—it demands integration into daily operations.
Operational Integration: Compliance policies cannot remain theoretical documents. The most common Privacy Rule failure involves treating HIPAA as a paperwork exercise rather than training staff to apply policies in real-world scenarios. This gap leads to accidental disclosures.
Security Rule Priorities
Three Security Rule elements require foundational attention:
Enterprise-Wide Risk Analysis: Risk assessments must extend beyond electronic health record systems to encompass the entire organizational infrastructure. OCR’s enforcement work consistently reveals this as a key deficiency. The agency has launched a dedicated Risk Analysis Initiative following a 264% increase in reported large breaches involving ransomware since 2018.
Encryption Standards: While not explicitly mandated, encryption should be considered essential. Organizations declining to encrypt ePHI must thoroughly document their rationale. This documentation becomes critical during investigations.
Administrative Safeguards: Workforce training and other administrative controls carry equal importance to physical and technical safeguards. Compliance represents a synergistic process requiring robust policies and procedures across all domains. Technology purchases alone—whether firewalls, EHR systems, or third-party certifications—do not constitute compliance.
The Certification Myth
Organizations frequently encounter “HIPAA-compliant” badges, shields, and certificates offered by vendors. These represent marketing materials, not evidence of compliance. No government-recognized HIPAA certification exists, and OCR has repeatedly stated that private seals create no safe harbor.
At best, these badges reflect point-in-time assessments by third parties. At worst, they generate false security for both organizations and patients. Covered entities remain responsible for conducting their own risk analyses, executing proper business associate agreements, and ensuring vendor controls match their specific environment. HIPAA compliance represents an ongoing process throughout an organization’s ecosystem, not a one-time achievement.
Budget Realities for Compliance Programs
HIPAA compliance costs vary significantly based on organization size, system complexity, and existing security infrastructure. While no official budget percentage exists, most small and mid-sized healthcare organizations allocate roughly 3-7% of operating budgets to Security Rule and HITECH requirements.
Typical investment ranges include:
- Enterprise-Wide Risk Analysis: $5,000-$20,000, depending on scope and whether technical testing is included
- Security Rule Remediation: $10,000-$100,000+, with policies and procedures forming the backbone that OCR examines rigorously during investigations
- Incident Response Planning: $3,000-$15,000 for customized tabletop exercises and planning
- Annual Training: $20-$50 per employee or $1,000-$5,000 for tailored sessions
Most SMBs face basic compliance startup costs in the low five figures. A single breach typically costs ten times that amount, making compliance investments comparable to insurance expenses.
Breach Notification: Communication Strategy Matters
Effective breach notification requires three elements:
Timeliness: Delays compound both regulatory and reputational harm. OCR opens investigations for every breach affecting 500 or more individuals, and increasingly investigates smaller breaches involving repeat offenders.
Clarity and Completeness: Patients and regulators need plain-language explanations covering what happened, what it means for affected individuals, and what remediation steps are underway. Industry-standard breach notifications often rely on legalistic tone, reactive posture, minimal detail, and generic templates.
Transparency: Patients deserve full disclosure of breach scope, including whether data has appeared on the dark web. Phrases like “we take privacy seriously” or “out of an abundance of caution” ring hollow. Organizations must acknowledge responsibility directly rather than deflecting blame.
Legal counsel plays an important role, but compliance and communication requirements remain distinct from legal privilege. Organizations should align legal and communications strategies while ensuring regulatory requirements are met. Transparency and integrity must guide communications even when attorneys recommend limiting disclosures.
Enforcement Landscape and Trends
OCR enforcement extends beyond monetary penalties to include corrective action plans and ongoing monitoring requirements. The HITECH Act also granted State Attorneys General authority to bring civil actions on behalf of residents, creating additional enforcement channels.
Recent developments include:
Media-Based Investigations: OCR regularly opens investigations based on public breach reporting, not solely on formal reports submitted through official channels. This underscores the importance of prompt, accurate disclosure.
Enforcement Initiatives: Following the Right of Access Initiative, OCR launched a Risk Analysis Initiative in fall 2024, with seven enforcement actions announced since. These targeted initiatives signal compliance priorities.
Organizational Changes: The closure of six HHS regional offices has reduced local investigatory capacity while the Office of the General Counsel actively recruits for its Health Data Branch, suggesting increased centralization of HIPAA enforcement work.
Regulatory Updates: The January 6, 2025 HIPAA Security Rule Notice of Proposed Rulemaking aims to strengthen cybersecurity requirements for ePHI. With final modifications potentially scheduled for May 2026, organizations may face just 240 days to achieve compliance following publication.
Action Plan for 2026
Healthcare organizations should prioritize these strategic investments:
- Conduct or update enterprise-wide risk analyses that examine all systems, not just EHRs
- Develop comprehensive policies and procedures integrated into daily operations
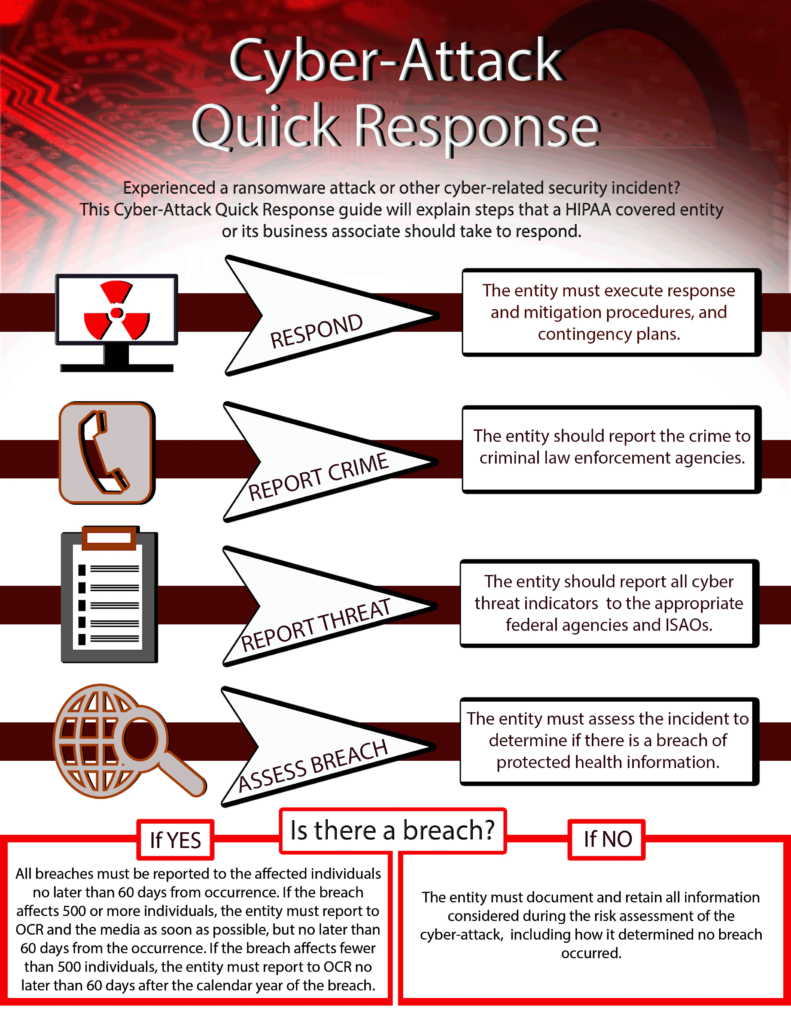
- Establish incident response capabilities including planning, routine monitoring, and tabletop exercises
- Implement workforce training programs that engage employees rather than treating training as a burden
- Strengthen vendor oversight through documented assessments and regular audits
- Review web properties for compliance with both Privacy and Security Rules
- Audit state law requirements to ensure compliance beyond federal minimums
- Prepare breach communication protocols emphasizing transparency and plain language
The regulatory environment continues to evolve, with proposed Security Rule modifications and new enforcement priorities emerging. Organizations that treat compliance as an ongoing process rather than a checkbox exercise position themselves to protect both patient data and institutional reputation.
For additional resources on HIPAA compliance, organizations can review materials available through the HHS Office for Civil Rights at hhs.gov/ocr and consult with qualified compliance professionals for organization-specific guidance.